In an era marked by growing and aging populations, healthcare systems worldwide face an increasing demand for acute care services. These services are crucial for addressing life-threatening emergencies, sudden flare-ups of chronic conditions, and a wide array of health issues requiring immediate attention. Integrating emergency interventions with primary care and public health initiatives is essential for building robust and effective health systems. This article delves into the meaning of acute care, its definition, and its significant role within the broader healthcare landscape.
Defining Acute Care Meaning: A Time-Critical Perspective
To foster meaningful discussions and guide the development of healthcare systems, clear definitions of health systems and services are paramount. According to the World Health Organization (WHO), health systems encompass all entities, institutions, and resources primarily aimed at promoting, restoring, and maintaining health.1 Health services, within these systems, are actions designed to improve health, diagnose, treat, and rehabilitate individuals. These services can be viewed as organized inputs for effective interventions, encompassing promotion, prevention, curative, rehabilitation, and palliative care, and can be directed at individuals or populations.1,2
Similarly, a precise definition of acute care is necessary. Medical definitions of acuity often emphasize the critical element of time sensitivity.3 Therefore, acute care services encompass all actions – promotive, preventive, curative, rehabilitative, or palliative, directed at individuals or populations – with the primary goal of enhancing health, where effectiveness hinges on timely, often rapid, intervention.
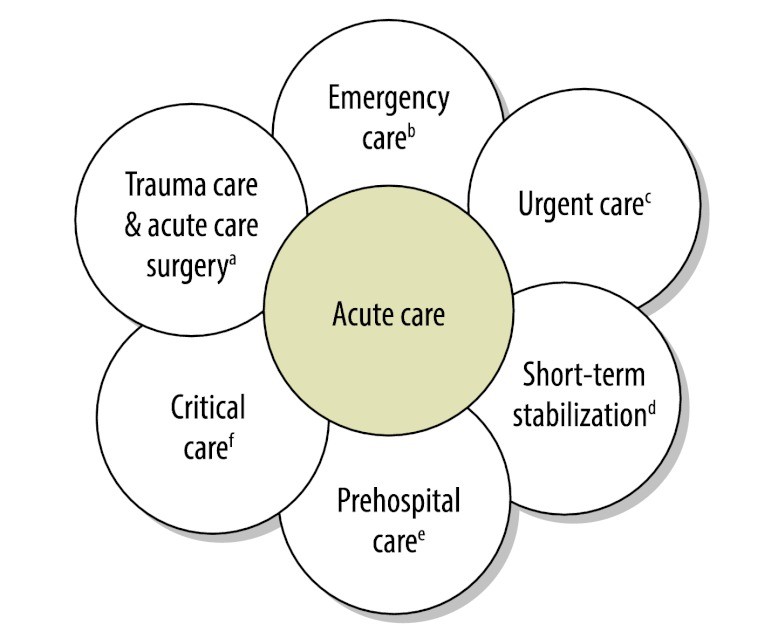
While many healthcare services benefit from timely delivery, acute curative services stand out as the most time-sensitive, irrespective of the specific illness. However, the concept of acute care has historically been poorly defined and under-supported in many developing healthcare systems. A practical working definition of acute care focuses on the most time-sensitive, individually-oriented diagnostic and curative actions aimed at improving health. A more comprehensive definition of Acute Care Meaning includes the health system components and care delivery platforms designed to manage sudden, often unexpected, urgent, or emergent episodes of injury and illness. These episodes, if not addressed swiftly, can lead to death or disability. The spectrum of acute care encompasses various clinical functions, including emergency medicine, trauma care, pre-hospital emergency care, acute care surgery, critical care, urgent care, and short-term inpatient stabilization, as illustrated in Figure 1.
Fig. 1. Domains within Acute Care Services
 Domains in acute care
Domains in acute care
Figure 1: This image illustrates the diverse domains encompassed by acute care, including surgical interventions for acute conditions, medical treatments for life-threatening illnesses, ambulatory care for walk-in patients, pre-definitive treatment stabilization, community-based emergency care, and intensive care for critically ill patients. Each domain highlights the time-sensitive nature and breadth of acute care services.
The Importance of Clearly Defining Acute Care Meaning: Addressing Health System Fragmentation
In 2007, the WHO underscored the urgency of strengthening health systems, yet precise definitions and objectives, particularly concerning health service delivery, often remain unclear.4 Priority health issues are typically identified through consensus lists developed by countries with input from international organizations. Subsequently, health services are structured to prevent and manage these prioritized health problems. However, a critical element often overlooked is the influence of time on the effectiveness and implementation of interventions.
Preventive strategies primarily aim to lower the likelihood of new cases by reducing disease risk factors. The earlier prevention efforts commence, the quicker the decline in disease incidence. Conversely, curative strategies focus on reducing disability or mortality among existing cases. The priority given to curative interventions depends on their time-sensitivity, effectiveness, and cost. In curative services, the relationship between time and effectiveness is crucial, emphasizing the need to ensure patients receive the right intervention at the right place and time. Neglecting the time-sensitive aspect of curative services leads to fragmentation through poorly coordinated care and ineffective application of clinical interventions. For instance, delays in antibiotic treatment for sepsis can result in death or disability. Such fragmented care reduces the potential to avert disability-adjusted life years (DALYs) with available resources.
Acute Care’s Contribution to Integrated Healthcare: A Holistic Approach
Acute care, as a clinical service, addresses immediate threats to life or limb, irrespective of the underlying cause. It inherently supports the development of robust health systems (a horizontal approach) rather than fragmented efforts that may improve outcomes for specific conditions but not the overall system functionality (vertical programs). Notably, the resources—material, consumable, and human—required for acute care platforms often overlap with those used in traditional “disease-centered” programs. It is crucial to dispel common misconceptions about acute care, such as equating it solely with ambulance services or high-technology dependence. Effective acute care is fundamentally driven by the temporal element – responding swiftly to immediate threats to life or limb – and involves strategic resource allocation to minimize impending death and disability. Integrating acute care with preventive and primary care completes a holistic healthcare system paradigm that encompasses all essential facets of healthcare delivery.
The conventional framework for categorizing health problems divides them into communicable diseases, noncommunicable diseases, and injuries. The ongoing global discussion on noncommunicable diseases highlights how care can become fragmented when the time sensitivity of curative interventions is disregarded. In 2008, noncommunicable diseases accounted for 63% of the 57 million deaths worldwide.5 A significant and growing proportion of deaths from noncommunicable diseases and injuries occur in low- and middle-income countries undergoing epidemiological transitions.6 Strategies to combat morbidity and mortality from noncommunicable diseases have predominantly focused on prevention and primary care. For example, guidelines for managing diabetes in primary health care in low-resource settings largely emphasize prevention. 7 However, only a few recommendations address time-sensitive measures, despite conditions like diabetic ketoacidosis being acutely life-threatening. The essential contribution of acute care in reducing the escalating burden of disease and injuries has been significantly underestimated.
Acute care plays a vital role in preventing death and disability, a role that primary care is often not equipped to fulfill. Within health systems, acute care also functions as a crucial entry point for individuals facing emergent and urgent health conditions. A clear definition of acute care meaning facilitates the development of metrics to evaluate acute care services, assess the disease burden they address, and set goals for advancing acute care, especially in low- and middle-income countries.8 The currently fragmented specialty areas within acute care have struggled to drive international growth in their respective clinical domains, partly due to a lack of appropriate metrics and coordinated health service delivery. Understanding acute care as an integrated care platform allows these disparate areas to unite under a single agenda and move forward cohesively.
Essential Next Steps for Strengthening Acute Care Globally
Many straightforward, effective, and affordable acute care interventions can be life-saving, often within the critical first 24 hours. These include interventions provided in basic surgery wards in district hospitals, addressing trauma, high-risk pregnancies, and other common surgical emergencies.9,10 Progress in recognizing and promoting acute care is evident through initiatives like the African Federation for Emergency Medicine (established in 2009) and the Academic Emergency Medicine Consensus Conference focused on global health and emergency care research. However, further crucial steps are needed to advance acute care development:
- Developing an acute care service delivery model tailored for low- and middle-income countries, operating in conjunction with preventive and primary services. These acute care services should address both life-threatening and limb-threatening conditions, as well as acute exacerbations of prevalent noncommunicable diseases.
- Enhancing coordination among acute care service providers, such as emergency physicians, surgeons, and obstetricians, to ensure efficient and effective delivery of critical acute care services.
- Establishing research methodologies to quantify the burden of acute care related diseases and injuries, including health economics and cost-effectiveness analyses, to justify the integration of acute care within health systems.
- Fostering national and international dialogues to promote better integration of acute care into local and national health systems.
This article serves as a call to action for leaders, policymakers, and academics to recognize the pivotal contribution of acute care systems in managing patients with communicable and non-communicable diseases and injuries. However, the development of such systems should not be misused as justification for diverting resources to under-resourced and poorly managed health facilities. Aligning key stakeholders, both nationally and internationally, to support the optimal balance of acute and preventive services is an urgent priority for health systems and society to effectively address the growing global disease burden.
Acknowledgements
The authors extend their gratitude to Linda J Kesselring for her invaluable assistance.
Funding:
JM Hirshon received funding from the National Institutes of Health Fogarty International Center (Grant 5D43TW007296).
Competing interests:
None declared.
References
[1] World Health Organization. Everybody’s business: strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva: World Health Organization; 2007.
[2] Frenk J. The health system and the public’s health: a conceptual framework. Bull World Health Organ 1993; 71: 117–23.
[3] Parrillo JE. Special report: recommendations for critical care training for physicians in multiple specialties. Crit Care Med 2006; 34: 304–05.
[4] World Health Organization. Health systems strengthening. Geneva: World Health Organization; 2009.
[5] World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization; 2009.
[6] Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 1997; 349: 1269–76.
[7] World Health Organization, International Diabetes Federation. Prevention and control of noncommunicable diseases: guidelines for primary health care in low-resource settings. Geneva: World Health Organization; 2012.
[8] Mock CN, Joshipura M, Goosen J, Kobusingye O, Nguyen S, Arreola-Risa C, et al. Strengthening care for the injured in developing countries: a case for integration into existing health services. World J Surg 2004; 28: 1249–55.
[9] McCord C, Chowdhury Q. Tools for operations research of district hospitals. Geneva: World Health Organization; 2003.
[10] Dare AJ, Walker IA, Hayes RJ, Cairns BA, Kayange NM, Mduma ER, et al. Trauma outcome in district hospitals in Tanzania. Injury 2007; 38: 30–37.