For professionals in the medical field, grasping the concept of the “Standard Of Care” is not just academic—it’s fundamental to responsible practice and mitigating legal risks. This article delves into the intricacies of this crucial benchmark, clarifying its definition, relevance, and determination, particularly in the context of medical malpractice and emergency situations.
What Exactly is the Standard of Care?
The standard of care is fundamentally a legal term, not a clinical one, although it profoundly impacts medical practice. It essentially defines the level of competence and caution expected of a healthcare professional when providing care. Think of it as the benchmark against which a clinician’s actions are measured to determine if their professional duties to patients have been adequately fulfilled. Failing to meet this standard is considered negligence, a serious matter with significant repercussions for clinicians.
The specific definition of the standard of care is legally determined by state entities—legislatures, administrative bodies, and courts—meaning it can slightly vary from state to state. However, the overwhelming majority of states adhere to a national standard. A clear example is found in Connecticut Code §52-184c, which describes it as: “…that level of care, skill and treatment which, in light of all relevant surrounding circumstances, is recognized as acceptable and appropriate by reasonably prudent similar health care providers.”
While most states have embraced the national standard, a few still operate under a locality standard. This might be defined based on the care provided within the same community, a similar community, or even the entire state. In some instances, a hybrid approach is adopted, applying the same or similar community standard for general practitioners but the national standard for specialists. Given the widespread access to information and expert consultation via the internet and telehealth, current risk management best practices strongly advise clinicians to strive to meet the national standard of care.
It’s crucial to understand that the standard of care is not synonymous with optimal care. Instead, it exists on a spectrum, ranging from just-acceptable care to the very pinnacle of medical excellence. In the context of medical malpractice litigation, the legal threshold is simply meeting the standard of care, even if it’s closer to the “barely acceptable” end of the spectrum. Naturally, from the perspective of patient well-being and achieving the best possible clinical outcomes, clinicians should always aim for optimal care.
Furthermore, the standard of care inherently acknowledges the importance of physician discretion and clinical judgment. These elements are vital components of patient care. Therefore, it is paramount for physicians to meticulously document their clinical reasoning and decision-making processes. This documentation serves as a clear record of the treatment rationale, invaluable for future caregivers and, if necessary, for expert witnesses in potential legal proceedings.
Relevance of the Standard of Care in Clinical Practice
The standard of care’s primary relevance to clinicians is in the realm of medical malpractice lawsuits. For a plaintiff to succeed in a malpractice claim, they must convincingly demonstrate four key elements:
- Duty: The clinician had a professional obligation to adhere to the standard of care for the patient (the plaintiff).
- Negligence: The clinician’s actions or omissions fell below the accepted standard of care.
- Harm: The patient experienced harm—whether physical, emotional, or financial.
- Causation: A direct causal link exists between the clinician’s failure to meet the standard of care and the harm suffered by the patient.
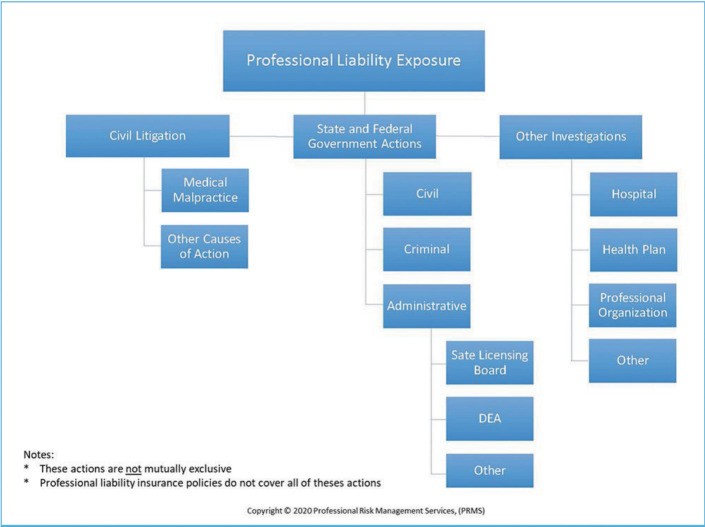
It’s important to note that the standard of care is specifically relevant to medical malpractice actions. Clinicians face various potential liability actions, as illustrated in Figure 1, where medical malpractice is just one category among others.
Figure 1. Professional Liability Exposure
Significantly, the standard of care—defined by the actions of reasonably prudent similar healthcare providers in comparable situations—is not pertinent in government investigations. In such inquiries, the focus shifts from comparing a clinician’s actions to peer practice to determining whether the clinician strictly adhered to the relevant laws and regulations, irrespective of what other professionals might be doing.
Determining the Standard of Care
Establishing the applicable standard of care in any clinical scenario involves considering a range of factors. These factors, ordered from most to least influential, include:
- Statutes: Federal and state laws, such as regulations governing prescription practices.
- Regulations: Federal and state administrative rules, for example, confidentiality mandates like HIPAA.
- Court Opinions: Judicial decisions that establish legal precedents, such as rulings on the duty to warn in cases involving potentially dangerous patients.
- Other Regulatory Statements: Guidelines and pronouncements from federal and state regulatory bodies, such as licensing boards.
- Authoritative Clinical Guidelines: While clinical guidelines themselves do not constitute the standard of care, they are significant factors used to determine it. Adhering to guidelines does not automatically prevent a finding of negligence, and conversely, deviating from them does not automatically equate to negligence. However, if established clinical guidelines (not utilization review guidelines) are not followed, the clinician should meticulously document the rationale and clinical judgment behind the deviation.
- Policies and Guidelines from Professional Organizations: Recommendations and standards set forth by reputable professional bodies like the American Psychiatric Association (APA) or the American Academy of Child and Adolescent Psychiatry (AACAP).
- Journal and Research Articles: Published peer-reviewed research and clinical findings in reputable medical journals.
- Accreditation Standards: Standards set by accrediting bodies for healthcare facilities and organizations.
- Facility Policies and Procedures: Internal protocols and guidelines established by the healthcare facility where the clinician practices.
In medical malpractice litigation, both the plaintiff and defendant will typically present expert witnesses. These experts analyze the factors listed above, alongside their own clinical expertise, to provide testimony on what they believe constitutes the applicable standard of care in the specific case. Ultimately, the fact-finder—the jury, or the judge in a bench trial—determines which expert’s interpretation of the standard of care is most credible and persuasive.
The Standard of Care in Emergency Situations
Contrary to potential assumptions, there is no distinct “emergency standard of care” needed for disasters or public health emergencies. The existing definition of the standard of care is inherently flexible. As previously discussed, it is defined as what a reasonably prudent similar healthcare provider would do under similar circumstances. This built-in flexibility allows the standard of care to be appropriately adapted to the unique and often challenging conditions presented by emergencies or disasters. The “circumstances” in the definition inherently include the context of an emergency.
Conclusion: Maintaining the Standard of Care
The most effective risk management strategy for clinicians is to proactively maintain their knowledge and skills in line with the evolving standard of care. This involves staying informed about the various factors that define the standard of care, including statutes, regulations, clinical guidelines, and professional best practices. By consistently doing so, clinicians can confidently demonstrate that they have met their professional obligations to their patients, should they ever face a medical malpractice claim.
Reference
[1] Connecticut General Statutes § 52-184c.